There is no cure for multiple myeloma. But several kinds of chemotherapy drugs can control the disease and improve your quality of life.
MSK often combines a few drugs to get the best treatment results. Using a combination of drugs can improve how well your treatment works.
Drugs work in different ways. We choose the type of chemotherapy drugs based on many things. They include how fast the cancer is growing, the role of genetic changes, and your general health.
Chemotherapy drugs for multiple myeloma
Chemotherapy (chemo) uses a drug or combination of drugs to kill cancer cells or slow their growth. It’s sometimes called systemic therapy because these drugs spread throughout your body.
Your MSK care team includes medical oncologists (cancer doctors) who will plan your chemotherapy treatment. You can get chemotherapy orally (swallowing medication) or intravenously (in your veins).
Chemotherapy drugs for multiple myeloma are:
- Melphalan (Alkeran®)
- Doxorubicin (Adriamycin® or Rubex®)
- Cyclophosphamide (Cytoxan® or Neosar®)
Chemotherapy drugs often are given with dexamethasone, a corticosteroid.
Side effects of chemotherapy drugs for multiple myeloma
Combining several drugs can raise the chance of side effects, including:
- Nausea (feeling like throwing up).
- Fatigue (feeling very tired).
- Rashes.
- More serious conditions, such as shortness of breath and seizures.
MSK researchers are exploring the best drug combinations. The standard treatment is to first weaken the disease. Most people will have primary therapy during outpatient visits.
If you’re eligible, after the standard treatment, you will have intensification (in-TEN-sih-fih-KAY-shun) therapy. This is treatment given after your primary therapy to kill any cancer cells that are left.
After this intensive phase of treatment, most people start maintenance treatment. It’s often with just 1 drug.
Proteasome inhibitors (PI) for multiple myeloma
Chemotherapy drugs are one class of drugs we use to treat multiple myeloma. Another class is called proteasome inhibitors (PI).
What are proteasomes?
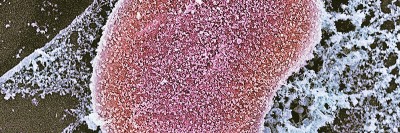
A proteasome is a large group of enzymes. It helps break down proteins that are no longer needed or are damaged. Both normal and myeloma cells have proteasomes.
What are proteasome inhibitors and how do they work?
A proteasome inhibitor blocks how cells get rid of proteins that are no longer useful. This causes proteins to build up, and then cells die. Myeloma cells seem to be more sensitive to proteasome inhibitors, and that’s why they die. But some healthy cells can die, too.
Proteasome inhibitor drugs
Bortezomib
The work of MSK researchers helped lead to the approval of the drug bortezomib (Velcade®). It’s a first-line treatment for multiple myeloma, often used together with other drugs.
Carfilzomib
Carfilzomib (Kyprolis®) is another first-line therapy, combined with lenalidomide and dexamethasone. Carfilzomib can work well when bortezomib or other treatments have not. It’s also used for multiple myeloma that has come back after treatment.
Ixazomib
Another drug is ixazomib (Ninlaro®), the only proteasome inhibitor that can be given by mouth. We usually combine ixazomib with other drugs.
Proteasome inhibitor side effects
Proteasome inhibitors can cause nerve problems, called neuropathy (noor-AH-puh-thee). Bortezomib is more likely to cause neuropathy than ixazomib or carfilzomib. Before you start treatment with proteasome inhibitors, you must take acyclovir, a drug that prevents herpes zoster (shingles).
Other drugs
Other drugs block the actions of certain proteins that myeloma cells need to live and grow.
Exportin (XPO1) inhibitors: What they are and how they work
Normal cells have a protein called XPO1 that moves materials in and out of the cell’s center. Changes in the XPO1 protein can cause cancer. Myeloma cells make too much XPO1, so cells can’t fight cancer.
Selinexor (Xpovio®) is a pill that can stop XPO1 from harming healthy cells. This slows the growth of myeloma cells and kills them.
BCL-2 inhibitors: what they are and how they work
Some kinds of myeloma cells make too much of a protein called BCL-2. This makes it harder for your body to tell the cells to die.
Venetoclax (Venclexta®) is a BCL-2 inhibitor pill that targets and blocks BCL-2 so your body can kill myeloma cells.
Immune-modifying drugs (IMiDs) for multiple myeloma
Immune-modifying drugs (IMiDs) work by helping your immune system recognize and kill myeloma cells. They also stop myeloma cells from growing in your bone marrow.
Immune-modifying drugs are pills. They often are combined with another drug, such as dexamethasone.
Most common immune-modifying drugs for multiple myeloma
Lenalidomide (Revlimid®)
Lenalidomide is a stronger form of thalidomide, with fewer side effects. Lenalidomide is the most common immune-modifying drug. It’s often used as a first treatment and for maintenance.
Thalidomide
Thalidomide treats multiple myeloma that has just been diagnosed. It also is used during maintenance to keep the disease from returning, or when it comes back after treatment.
Pomalidomide (Pomalyst®)
Pomalidomide is a newer IMiD for multiple myeloma. It’s used when lenalidomide and other drugs stop working.
Side effects of multiple myeloma immune-modifying drugs
Lenalidomide and pomalidomide can cause a blood clot (thrombus) in your legs. During your treatment with either drug, you must take a blood thinner to prevent blood clots.
Another risk with this class of drugs is birth defects. We will enroll you in a program before you start treatment with lenalidomide or pomalidomide. The Risk Evaluation and Mitigation Strategy (REMS) drug safety program follows federal guidelines.
We’re available 24 hours a day, 7 days a week