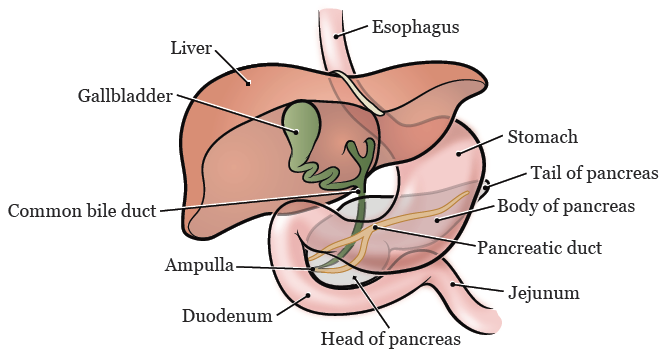
What the pancreas looks like and its anatomy in your body
Most pancreatic cysts are benign (not cancer) and have a low chance of causing harm or symptoms. But some are precancerous, which means they can become pancreatic cancer. It’s important to find out what type of cyst you have.
Pancreatic cysts are growths filled with fluid that grow in the pancreas, a small gland. It’s located in your abdomen (belly) between your stomach and intestines.
The main job of the pancreas is to make enzymes, a kind of protein that helps you digest food. These enzymes are made by a type of cell called an exocrine cell. Endocrine (islet) cells make 2 hormones, insulin and glucagon. They help control blood sugar levels in your body.
Sometimes pancreatic cysts grow as a result of pancreatitis (PAN-kree-uh-TY-tis), an inflammation of the pancreas.
But most start for other reasons. We find them by chance during a CT or MRI scan done for another purpose.
MSK uses the latest imaging methods, new technology that can find many more cases of pancreatic cysts.
Types of pancreatic cysts
There are nearly 20 types of pancreatic cysts. Here are common pancreatic cysts:
Pseudocysts
Pseudocysts (SOO-dow-sists) are mostly made of fluid. They can start in or near the pancreas. They often happen after acute pancreatitis, an inflammation of the pancreas. You are not likely to get pseudocysts if you have never had pancreatitis or a pancreas injury.
Serous cystadenomas (SCAs)
Serous cystadenomas (SEER-us sist-A-deh-NOH-muhs) have thick, fibrous walls and are filled with fluid. Almost all SCAs are benign (not cancer). But they can cause pain, jaundice, or make you uncomfortable as they grow.
Intraductal papillary mucinous neoplasms (IPMNs)
IPMNs start in the ducts that connect the pancreas to the intestine. They’re the most common type of cyst that can turn into cancer. They make large amounts of proteins that form mucus (mucin) in the cyst lining and fluid.
It’s hard to predict if and when an IPMN will become cancer. But research suggests IPMNs in the main pancreatic duct are at higher risk for turning into cancer.
Mucinous cystic neoplasms (MCNs)
These cysts are growths that can become cancer. They start in the body and tail of the pancreas. They’re almost always in women. Large MCNs have tiny walls that divide the cyst into compartments, called septations. They may be more likely to become cancer.
Monitoring pancreatic cysts
MSK’s Pancreatic Cyst Surveillance Program is one of the largest in the country. It monitors pancreatic cysts and has provided treatment more than 5,000 people. Each year, MSK sees more than 300 new patients who have a pancreas cyst.
Our pancreatic cyst specialists recommend that people diagnosed with cysts should be closely monitored.
MSK Pancreatic Cyst Surveillance Program is managed by our Hepatopancreatobiliary (HPB) Service. They’re experts in the treatment of pancreatic cysts and pancreatic, liver, and bile duct cancers. It’s a team of surgeons, pathologists, oncologists (cancer doctors), radiation oncologists, and nurse practitioners.
The program will monitor you throughout your life. It’s important to know you may still need ongoing monitoring even after we remove the cysts during surgery. That’s why we encourage people with cysts to join MSK’s Pancreatic Cyst Surveillance Program.
Pancreatic cyst research
As we try to understand why pancreatic cysts start, MSK also is working to define the best practices for caring for cysts. We’re finding the best ways to tell:
- Which cysts to remove right away.
- Which cysts could become cancer over time
- How to manage each type of cyst.
Our researchers are also exploring biomarkers, such as proteins and genes. They can help us know which cysts are benign (not cancer) or precancerous.
This information can help predict whether a precancerous cyst will turn into cancer. It guides decisions about monitoring and treatment.
Your care team may recommend a consultation with the experts who work on our Pancreatic Tumor Registry. This database helps us find pancreatic cancer early, when there are better treatments.
You may be able to join the registry if you have 1 or both of these:
- A family history of pancreatic cancer
- A genetic change (mutation or variant) that raises your risk for getting pancreatic cancer
We’re available 24 hours a day, 7 days a week


