The routine use of epidural analgesia for patients with non-small cell lung cancer (NSCLC) who undergo a minimally invasive lobectomy is not warranted, according to the results of our retrospective study published recently in the journal Lung Cancer.
We found no differences in preoperative, surgical, or pathological factors between patients with stages I to III NSCLC who underwent a minimally invasive lobectomy procedure with or without epidural analgesia. Moreover, the length of hospital stay was three days for patients who did not have epidural analgesia, one day shorter than for patients who did. (1)
A prospective study is required to confirm our findings and determine the safety of using alternative methods of acute postoperative pain management in this patient population. At present, our evidence makes a compelling argument against the routine use of epidural analgesia in this patient population.
As minimally invasive surgical approaches continue to become more common for lung cancer treatment, we will continue to question and redefine standard methods to ensure that we optimize patient outcomes and minimize the negative side effects of treatments.
Surgical Approach Shifts to More Minimally Invasive Procedures
Over the last decade, surgical practice has shifted to more minimally invasive surgical approaches for treating patients with early-stage NSCLC. Minimally invasive video- or robotic-assisted surgeries are associated with fewer postoperative complications, such as arrhythmias and pneumonia; less time requiring a chest drain; and a shorter hospitalization. (2), (3), (4), (5), (6), (7), (8)
Several national databases have reported better patient outcomes with minimally invasive surgery versus thoracotomy with regard to the rate of complications and (9), (10), (11), (12), (13), (14), (15) the length of hospital stay, (10), (12), (14), (16) with similar long-term survival. (13), (16), (17) Minimally invasive lobectomy is also associated with less pain during the acute postoperative period compared to thoracotomy. (5), (18)
Epidural Analgesia for Lobectomy
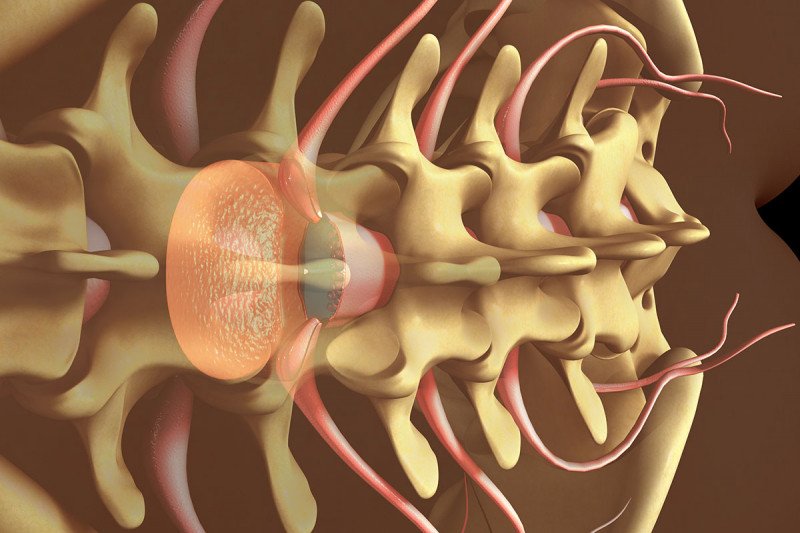
Optimizing perioperative analgesia to reduce the compromising effects of pain on postoperative respiratory function and patient morbidity is imperative. (19)
Epidural analgesia has traditionally been considered the gold standard for patients undergoing major open abdominal surgery and open thoracotomy. However, it is associated with several complications, including placement issues, and side effects, such as hypotension and urinary retention. (20), (21) In contrast, patients who received systemic analgesia alone are hospitalized for shorter periods and require smaller opioid dosages at discharge. (22)
Study Design
We examined the shift in the prevalence of the use of epidural analgesia and its impact on postoperative short-term outcomes after a lobectomy via minimally invasive surgery or via thoracotomy in patients with NSCLC. Using prospectively collected data from the Memorial Sloan Kettering Cancer Center Thoracic Surgery Service database, we identified 793 patients with stages I to III NSCLC who’d had a lobectomy procedure. (1)
To capture the shifts in surgical practice toward more minimally invasive surgeries, we divided the patients into two groups. The early group of 386 patients was treated between January 2009 and December 2010, and the late group of 407 patients was treated between January 2014 and December 2015. (1)
Within the late group of 308 patients who underwent minimally invasive surgery, we compared the results for 150 patients who received epidural analgesia with 158 patients who did not. (1)
Study Results
As expected, there was a clear shift toward the increased use of a minimally invasive surgical approach over time. In the early group, 53 percent had minimally invasive surgery, and 47 percent had a thoracotomy. By contrast, in the late group, 76 percent had minimally invasive surgery, and 24 percent had a thoracotomy. (1)
There were no differences in postoperative morbidity and mortality between the two time periods for both minimally invasive surgery and thoracotomy methods. (1)
Among patients who had a minimally invasive lobectomy, the use of epidural analgesia decreased significantly from 95 percent in the early time period to 51 percent in the late time period (p < 0.001). There were no differences in morbidity or mortality for patients who did or did not have epidural analgesia. (1)
Notably, the length of stay in the hospital was three days for those who did not have epidural analgesia compared to four days for those who did (p = 0.038). (1)
Advancing Lung Cancer Care
At MSK, we are dedicated to advancing lung cancer care through research. For example, since 2015, I have been leading an open-label, dose-escalating, nonrandomized phase I trial studying the use of genetically engineered chimeric antigen receptor (CAR) T cell therapy to treat mesothelioma and malignant plural disease from lung and breast cancers. The novelty of these studies includes administering CAR T cells regionally in the pleural cavity and combination immunotherapy with pembrolizumab. The study is still recruiting at seven MSK locations. We are awaiting regulatory approvals to initiate a phase II study.
MSK investigators are also conducting 67 other clinical trials for people with lung cancer, testing a range of new chemotherapies, targeted therapies, immunotherapies, and radiation therapies.
The study authors’ lab work is supported by grants from the National Institutes of Health (P30 CA008748, RO1 CA236615, and RO1 CA235667), the US Department of Defense (BC132124, LC160212, CA170630, and CA180889), the Emerson Collective Cancer Research Fund, the Derfner Foundation, the Joanne and John DallePezze Foundation, William and Alice Goodwin, the Commonwealth Foundation for Cancer Research, and the Center for Experimental Therapeutics at MSK. None of the funding sources had any role in the study design; in the collection, analysis, and interpretation of the data; in the writing of the report; or in the decision to submit the article for publication.
