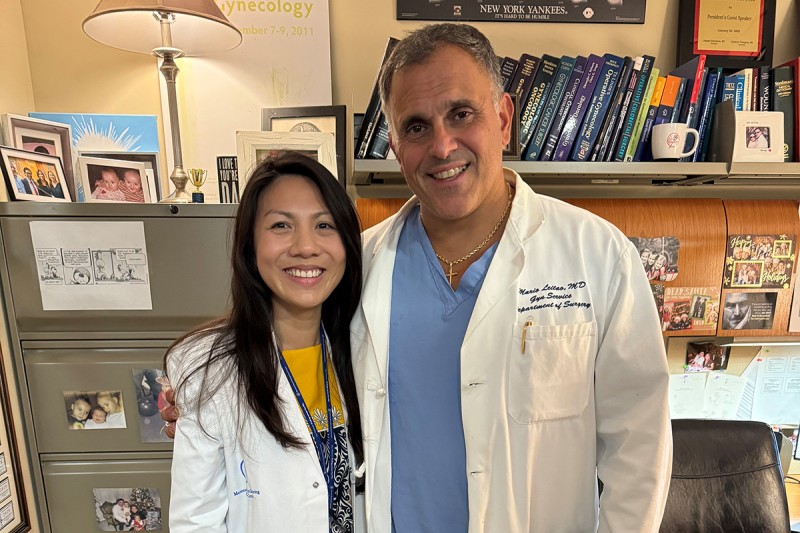
Dr. Anh Le had a lethal form of cervical cancer and needed complex surgery from gynecologic oncology surgeon Dr. Mario Leitao and a team of MSK experts. Nearly five years later, she reunited with Dr. Leitao during a one-month surgical residency rotation at MSK.
Anh Le had begun her second year of medical school in Chicago, in 2018, when she suddenly faced her own health emergency: a rare, deadly form of cervical cancer called glassy cell carcinoma. The diagnosis threw her life — and promising career — into turmoil.
It also set her on a path that brought her to Memorial Sloan Kettering Cancer Center (MSK) under two profoundly different circumstances — first as a patient and then as a doctor in training to treat gynecologic cancers like hers.
“I cannot emphasize enough how MSK has been an incredibly monumental place, both in saving my life and shaping who I am today,” Dr. Le says.
At first, doctors in Chicago tried to stop the disease with a hysterectomy, chemotherapy, and radiation, including brachytherapy. But a year later, the cancer returned in multiple spots in her pelvis. The outlook was dire — the five-year survival rate for someone with a recurrence of this cancer was less than 50%.
Her doctors said her only hope was a total pelvic exenteration — a major surgery that removes all organs in the pelvis, including the ovaries, bladder, rectum, anus, urethra, and vagina. She would permanently have external tubes for eliminating solid waste and urine. She would lose her fertility at age 30. The news was devastating.
“I had assumed that if there was another recurrence of my cancer, it would just mean longer chemotherapy,” Dr. Le says. “I was in shock that I needed surgery that would be so extensive and life changing.”
Choosing Pelvic Exenteration Surgery Experts for Her Glassy Cell Carcinoma
Her situation was desperate, and Dr. Le took no chances when researching the best treatment for glassy cell carcinoma. A mentor in her home state of Arizona suggested she seek a second opinion at MSK. Dr. Le came to New York City and met with MSK gynecologic medical oncologist Angela Green, MD, and gynecologic surgeon Mario M. Leitao, Jr., MD.
Dr. Le hoped they would tell her she didn’t need the exenteration, but they were in firm agreement: It was by far the best option for saving her life.
As a doctor herself, she understood the number of times a surgeon has performed a surgery is crucial. The fact that Dr. Leitao had done an exenteration multiple times gave her confidence. What’s more, MSK was the very first hospital to perform this surgery back in the 1940s, by MSK’s first Chief of Gynecology, Dr. Alexander Brunschwig.
“Looking back, I don’t think I could have been where I am today with any doctor but him,” she says, her voice choking with emotion. “Everyone at MSK has been amazing, but Dr. Leitao holds a very special place for me.”
Another reason Dr. Le chose MSK: Her care team would include a range of specialists to handle different parts of the complex surgery. The procedure would require not only removing the cancer but also constructing new ways to divert urine and solid waste, as well as reconstructing part of the vagina.

MSK caregivers were always by Dr. Le’s side, helping her recover after the major surgery.
“I felt more comfortable with three teams being very good at their specific parts of the procedure, rather than one surgeon doing the entire thing,” she says.
In November 2019, she underwent the operation, which required exquisite coordination:
-
Dr. Leitao, working with one of his partners, gynecologic surgeon Vance Broach, MD, removed the glassy cell carcinoma by doing the pelvic exenteration. They also created a permanent colostomy from the bowel for eliminating waste.
-
Urologic surgeon Bernard H. Bochner, MD, created a new bladder by forming a pouch from a portion of the colon and a section of the small intestine. This allowed urine to be diverted from the body at regular intervals through a catheter.
- Plastic and reconstructive surgeon Babak J. Mehrara, MD, recreated a vaginal cavity using muscles from Dr. Le’s thighs.
“It went better than expected,” Dr. Le says. “They thought it would take up to 12 hours and that I would have to have a breathing tube for at least a day after the surgery, but I was out of the operating room within seven hours with no tube when I woke up.”
After Surgery, More Treatment to Stop Recurrence
The MSK doctors knew lingering cancer cells could still pose a serious threat. As Dr. Le was recovering in New York over the next two months, a CT scan showed an enlarged lymph node in her right groin. Dr. Leitao removed that node and a few surrounding ones.

Dr. Le with her parents at graduation from medical school.
Tests showed the node did indeed contain cancer cells.
Dr. Le conferred with Dr. Leitao who recommended she have immunotherapy with a drug called pembrolizumab (Keytruda®). After returning to Chicago, Dr. Le received this treatment under the care of a local physician once every three weeks for two years.
Remarkably, through her entire experience, Dr. Le never took a leave of absence from medical school. After her initial diagnosis, she juggled a hysterectomy, chemotherapy, radiation, and brachytherapy, only taking sporadic days off. As she recovered from her surgery at MSK, she took online courses that most medical students save for their fourth year.
Helping Cervical Cancer Patients Like Her
Dr. Le first become interested in gynecologic oncology when she was diagnosed. The recurrence convinced her this path was her destiny.
“Having experienced all that I did, I was sure these were the people I wanted to care for,” she says. “It made me realize how many gaps in healthcare exist for gynecologic oncology patients, particularly from an emotional perspective. I want to be able to give back to those patients.”
There is a pressing need for this expertise. Despite cervical cancer being widely viewed as preventable due to the HPV vaccine, not enough women are receiving it. A 2025 report from the American Cancer Society showed an increase in new cases of cervical cancer among women 30 to 44. (The incidence has declined in younger women.)
Since finishing medical school, Dr. Le is now in her third year as an OB/GYN resident at Banner-University Medical Center in Phoenix.
In a full-circle moment, Dr. Le came back to MSK in July 2024 for a month of intensive training as part of the Gynecological Brunschwig Rotating Resident Program — named after the very doctor who developed the lifesaving procedure. She ended up training alongside two people who had assisted in her surgery five years earlier — Dr. Broach, and gynecologic surgeon Evan Smith, MD, who is now an assistant attending surgeon.

Dr. Le remains very active today, hiking and running half-marathons.
“The MSK gynecologic oncology team is absolutely amazing,” says Dr. Le. “It was truly special to be part of MSK, even if for only a month.”
Nearly five years after her surgery, Dr. Le has no evidence of cancer and is remarkably active, considering all she’s endured. She likes to hike, run half-marathons, and forage for mushrooms.
She may still be a trainee, but she has special wisdom.
“I would tell young adults in the same situation to understand that mourning the loss of the person you were before all this is okay,” she says. “It’s okay to be patient with yourself, that it’s a long journey and there’s going to be lot of hard days. Today I try my best to be in the moment, keep a positive attitude, and live with no regrets because everything can change in an instant.”
She keeps going by reminding herself of a quote from Jane Marczewski, a singer on America’s Got Talent and a breast cancer patient. Her words are Dr. Le’s mantra: “You can’t wait until life isn’t hard anymore before you decide to be happy.”




