This information describes what a blood clot is and how it’s treated.
Normal blood clots form in blood vessels when a clump of platelets (a type of blood cell) come together to stop bleeding when you have a cut or an injury. When the cut or injury heals, your body will get rid of the blood clot. Blood clots can form anywhere in your body.
Blood clots can also form in healthy blood vessels when they aren’t needed. This is called an abnormal (not normal) blood clot. Abnormal blood clots can lead to serious health problems.
Types of blood clots
There are 2 types of blood clots that can be dangerous: deep vein thrombosis and pulmonary embolisms.
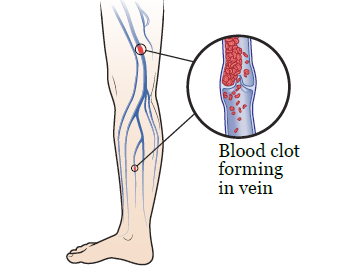
Deep vein thrombosis (DVT)
DVT can happen when an abnormal blood clot forms in a vein deep inside your body, usually in your arm or leg (see Figure 1). The clot may affect your normal blood flow and cause swelling, redness, and pain in the area. If the clot isn’t treated, new blood clots may form. The clot may also break apart and spread to other parts of your body. These things can make the swelling and pain worse and lead to trouble walking, an infection, or skin ulcers (sores).
Pulmonary embolism (PE)
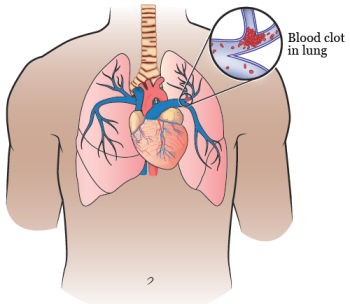
A PE can happen when an abnormal blood clot blocks the flow of blood in a blood vessel in your lung (see Figure 2). Most of the time, this happens when a blood clot in a deep vein of your leg breaks loose and travels to your lung. Having a PE can keep your body from getting enough oxygen.
If you have a PE, you may have:
- Trouble breathing
- Chest pain
- A fast heartbeat
- Pale or blue-colored skin
A PE can cause death if the signs aren’t treated quickly.
Blood clot risk factors
Some things can increase your risk of forming a blood clot. The risk factors include:
- Not moving around often. This is because blood will flow slower in your deeps veins when you’re not moving, which can lead to a clot.
- Having recently had surgery. This is because some surgeries may cause your blood to become thicker, or it may pool if you’re having a long surgery and not moving much.
- Having cancer
- Having a central venous catheter (CVC)
- Being hospitalized
- Being injured
- Pregnancy
- Taking birth control or hormone replacement therapy that contains estrogen
- Being overweight
- Family history of blood clot
- Smoking
While you’re in the hospital, you may have more than 1 of these risk factors at the same time.
Symptoms of blood clots
Blood clots can reduce the flow of blood throughout your body. Sometimes, people with a blood clot don’t feel any symptoms until the problem becomes life threatening.
Symptoms of these blood clots include:
- Sudden pain and swelling in 1 arm or leg
- Trouble walking due to swelling and pain
- Sharp chest pain
- Fast heartbeat
- Trouble breathing
- Severe abdominal (belly) pain with or without vomiting (throwing up) and diarrhea (loose or watery bowel movements)
- Pale or blue-colored skin
Call your healthcare provider right away if you notice any symptoms of a blood clot.
Diagnosing blood clots
Since some people don’t have any symptoms of blood clots, many blood clots are found when your healthcare provider is looking for something else, such as when you have an imaging scan. Make sure you tell your healthcare provider if you have any symptoms of a blood clot.
If your healthcare provider thinks you have a blood clot, they will recommend 1 or more of the following tests:
- A computed tomography (CT) scan of your lungs to look for a PE. A CT scan takes x-ray pictures of your internal organs.
- An ultrasound of your veins to look for blood clots in your legs or arms. The ultrasound machine uses sound waves to create pictures of the inside of your body.
- Blood tests to measure how quickly your blood clots. Blood tests can also see if you have any genes that may increase your risk blood clots.
Treating blood clots
Treatment for a blood clot usually includes taking a blood thinner, also known as an anticoagulant. This is the most common treatment for blood clots. Blood thinners help prevent your body from making new clots.:
Blood thinners can be given:
- By an injection (shot) into a vein or under the skin. Examples include Heparin, enoxaparin sodium (Lovenox®) and fondaparinux (Arixtra®).
- By mouth as a tablet. Examples include warfarin (Coumadin®), rivaroxaban (Xarelto®), apixaban (Eliquis®), and edoxaban (Savaysa®).
Your healthcare provider will decide which type of medication is best for you.
How long you’ll need to take blood thinners depends on many factors. Your healthcare provider will consider your risk factors and will help decide how long you need to take them. Some people may need to stay on them forever. You’ll have regular visits with your healthcare provider while you’re on blood thinners.
Some blood thinners may have special instructions, such as medications you’ll need to avoid while you’re taking them. If you’re taking a blood thinner with any special instructions, your healthcare provider will go over them with you.
Preventing blood clots
There are many things you can do to prevent blood clots from forming. The following are ways to prevent blood clots.
Physical activity
Staying active is a good way to prevent blood clots. Mild or moderate exercise (such as walking or yoga) can improve your blood flow. Try to move every few hours, if you’re able to, as instructed by your healthcare provider. For most people, this means as much as you feel comfortable with.
It’s also important to move often if you’re sitting for long periods of time, such as while traveling on a plane or in a car. If you’re unable to get out to walk around, be sure to change positions often while on a long trip.
If you’re not able to move around easily, try doing some light stretches and movements with your feet, if you’re able. You can make circles with your feet or point your toes up and down while you’re sitting or lying down.
Medication
If your healthcare provider prescribed you anticoagulation medication (blood thinners), be sure to take your medication as instructed. This medication will reduce the chance of a blood clot forming.
Sequential compression device (SCD) sleeves
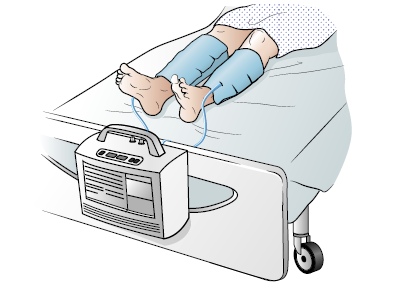
If you’re in the hospital, your risk of getting a blood clot is higher. To help prevent a blood clot, you can use SCD sleeves.
SCDs are sleeves that wrap around your lower legs (see Figure 3). The sleeves are connected by tubes to a machine that pushes air in and out of the sleeves to gently squeeze your legs. This is a safe and effective way to help your blood circulate (move around) to prevent clots.
You should always wear the SCD sleeves when you’re in your hospital bed, unless your healthcare provider tells you not to. Make sure you remove the SCD sleeves before getting out of bed, because the tubing could make you trip and fall. Tell your healthcare provider if you notice the tubing is pinched or the pump is beeping.
Other tips to prevent blood clots
You can also help prevent blood clots by following these tips:
- Wear loose-fitting clothes, socks, or stockings.
- If your healthcare provider recommends them, wear compression stockings. These are special stockings that can improve your blood flow.
- Avoid crossing your legs while sitting.
- Raise the bottom of your bed 4 to 6 inches with blocks or books. This will help elevate your legs to improve your blood flow.
- Eat less salt. Eating too much salt may cause swelling and can increase your risk of getting a blood clot.
When to call your healthcare provider
Call your healthcare provider if you have:
- Increased pain, swelling, or both in the arm or leg with the blood clot
- New pain, swelling, or both in your other arm or leg
- Trouble breathing
- Severe headaches or headaches that don’t go away
- Nose bleeds
- Bleeding gums
- Blood in your urine (pee), stool (poop), vomit, or in the mucus that you cough up through your mouth
- A heavier menstrual flow (period) than usual
- Bleeding that doesn’t stop
- Bruising that doesn’t go away
- Fallen or hurt yourself in any way
- Plans for any dental procedure or surgery
- Stopped taking your blood thinner for any reason
- Any unexpected, unexplained side effects
- Any questions or concerns